Esophageal High-Resolution Manometry in Gastroesophageal Reflux Disease
22-year-old man presented with 10 years of retrosternal burning and suspected gastroesophageal reflux. Despite taking omeprazole (20 mg once daily) 30 minutes before breakfast, avoiding foods that precipitated symptoms, and sleeping with his head elevated, heartburn and regurgitation while supine continued. He reported intermittent solid-food dysphagia for 2 years but no weight loss (254-lb [115 kg] body weight); physical examination results were unremarkable.
Esophagogastroduodenoscopy (EGD) revealed normal esophageal mucosa and normal biopsies. Given his persisting symptoms, an esophageal high-resolution manometry (HRM) study was performed (Table 1; eFigure in the Supplement).
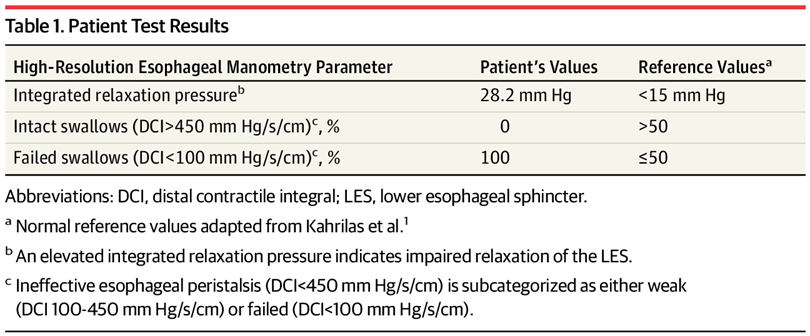
Patient Test Results
What Would You Do Next?
- Perform 360-degree (Nissen) fundoplication.
- Perform esophageal (Heller) myotomy and partial fundoplication.
- Increase omeprazole dosing to twice daily.
- Replace omeprazole with nortriptyline.
DiscussionAnswer
B. Perform esophageal (Heller) myotomy and partial fundoplication.Test Characteristics
GERD (gastroesophageal reflux disease) can present at any age. HRM is not necessary for most patients with GERD, but it is indicated for evaluating esophageal motor function in patients with persistent esophageal symptoms (dysphagia, heartburn, regurgitation) that are unresponsive to antireflux medication and are not explained by diagnostic testing with endoscopy or contrast radiography. HRM is also used to identify the location of the lower esophageal sphincter (LES) for positioning of ambulatory reflux monitoring catheters and for assessing esophageal peristalsis prior to fundoplication. In contrast to the 5 to 8 recording sites with conventional esophageal manometry, HRM uses a catheter embedded with 20 to 36 closely spaced circumferential pressure sensors inserted transnasally into the stomach, spanning the entire esophagus. Medications that can affect esophageal smooth muscle function (ie, calcium channel blockers, nitrates, metoclopramide, opioids) are stopped whenever possible. A standard HRM protocol typically involves 10 wet swallows (in which 5 mL of ambient temperature water is swallowed on cue).
Raw pressure data from each swallow are transformed by HRM software into topographic color-coded pressure contour plots (Clouse plots). Chicago Classification (version 3) describes esophageal motor function using 3 software metrics: integrated relaxation pressure (IRP; measures adequacy of LES relaxation for swallowed content to pass through), distal contractile integral (DCI; quantifies vigor of smooth muscle peristalsis), and distal latency (DL; identifies appropriate sequencing of peristalsis). An IRP of greater than 15 mm Hg has a sensitivity of 93% to 98% and a specificity of 96% to 98% for a diagnosis of achalasia (defined as lack of LES relaxation with absent or abnormal esophageal body peristalsis).
In 2018, Medicare paid $144.86 for HRM studies.Application of Test Results to This Patient
In this patient, HRM revealed absent esophageal peristalsis and median IRP of greater than 15 mm Hg (Table 1; eFigure in the Supplement), which indicated no LES relaxation with swallows, and a diagnosis of achalasia. Achalasia type II consists of failed LES relaxation resulting in obstruction at the esophagogastric junction and increased intraluminal pressure throughout the esophagus with swallows.
This patient with achalasia presented with symptoms similar to GERD. EGD was normal, and esophageal symptoms persisted despite acid suppressive therapy. In this setting, at least 30% of patients have alternate diagnoses, such as functional heartburn (heartburn without objective evidence of GERD, eosinophilic esophagitis, or major motor disorders), achalasia, or rumination syndrome (effortless, volitional postprandial regurgitation of undigested food from the stomach). As many as 2% to 3% of patients undergoing HRM prior to antireflux surgery have evidence of achalasia, when fundoplication without LES disruption will exacerbate obstruction from the incompletely relaxing LES.7 Therefore, HRM is important in the evaluation of persistent esophageal symptoms not responding to standard GERD therapy.
Although achalasia and GERD can present with similar retrosternal burning and/or regurgitation, management is different. Disruption of the LES (using graded pneumatic dilation, surgical myotomy, or per-oral endoscopic myotomy) effectively treats achalasia symptoms. In contrast, augmentation of the LES with fundoplication is useful when documented GERD persists, despite medical management. Establishing this distinction between achalasia and GERD is important prior to surgical intervention, and HRM establishes this distinction.Alternative Diagnostic Testing Approaches
When evaluating esophageal motor function, HRM is more accurate than conventional manometry in diagnosing achalasia. Conventional manometry may not identify abnormal LES relaxation if the recording sensors are not precisely positioned, potentially increasing cost from missed achalasia diagnoses. Esophageal HRM has largely replaced conventional manometry due to increased diagnostic accuracy, better reproducibility, and ease of interpretation.Table 2.
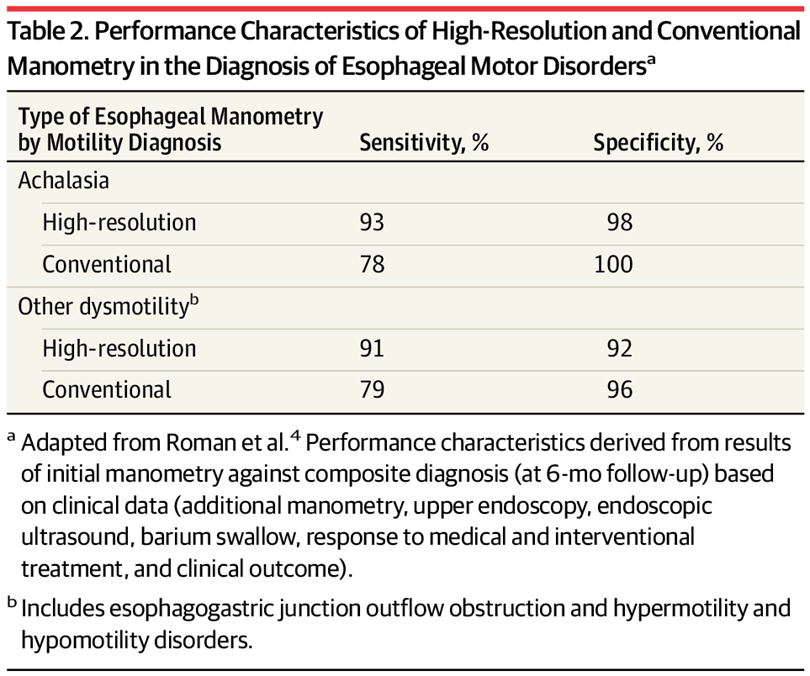
Performance Characteristics of High-Resolution and Conventional Manometry in the Diagnosis of Esophageal Motor Disordersa
EGD is integral to the evaluation of dysphagia and persistent heartburn to rule out mechanical obstruction (such as eosinophilic esophagitis, stricture, or malignancy), but EGD does not reliably assess esophageal motor function and only identifies achalasia in one-third of patients with the diagnosis. A timed barium swallow with barium column height of 5 cm at 1 minute has a sensitivity of 94% but a specificity of only 76% in diagnosing achalasia.Patient Outcome
This patient underwent an uncomplicated laparoscopic Heller myotomy with partial fundoplication. Eight years later, his heartburn, regurgitation, and dysphagia symptoms had resolved.
Clinical Bottom Line
- The differential diagnosis of proton pump inhibitor–nonresponsive heartburn and/or regurgitation symptoms includes GERD, esophageal motor disorders, eosinophilic esophagitis, rumination syndrome, and functional esophageal disorders.
- Esophageal HRM is useful for investigating esophageal symptoms that persist despite acid suppressive therapy and do not yield a diagnosis after EGD. HRM is also useful for evaluating esophageal peristaltic performance prior to fundoplication.
Source: AMA Wire